Part 3: Privatizing learning difference treatment
Private practices through the lens of students, providers, and payers
Part 2 detailed ‘The Public School Path’ for LD treatment and alluded to the role private practices play at this intersection of healthcare and education. Today, we’ll explore these practices through three lenses:
Students: What does the ‘Private Practice Path’ look like?
Providers: What is the private practice business model for LD treatment providers (known as educational therapists)?
Payers: How is private practice treatment financed by families?
Students
The Private Practice Path is taken by students in private schools or those in public schools whose families can afford it.
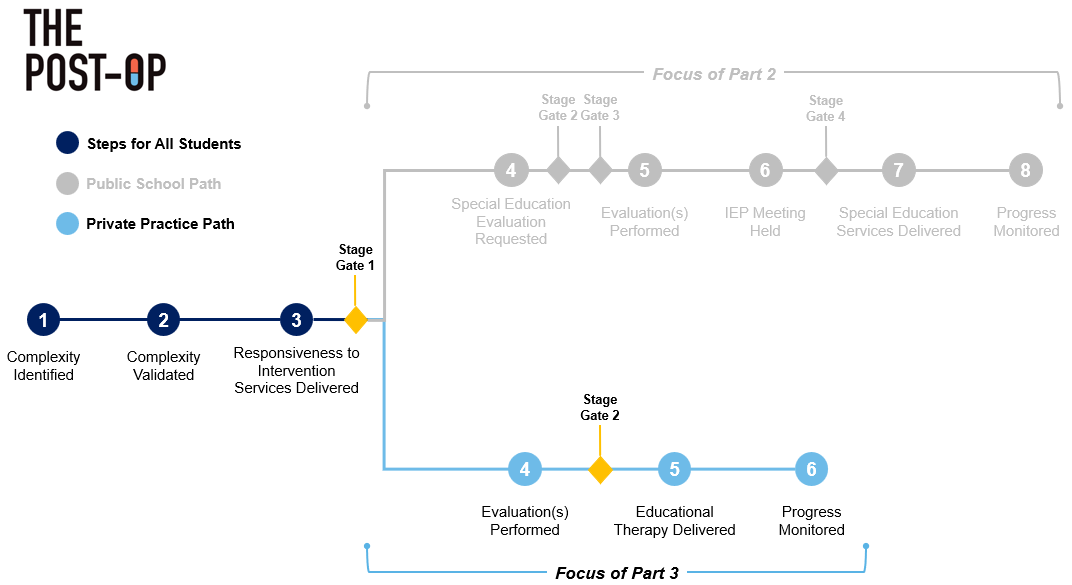
Chart 1: The divergent path of learning differences
Steps 1-3: Complexity Identified & Validated + RTI Services Delivered
These steps are similar regardless of the path taken. Refer to Part 2 for more details!
Step 4: Evaluation Performed
Using data gathered during RTI services, parents can seek a referral from the teacher to receive an evaluation from a privately practicing neuropsychologist, costing anywhere from $1,500-$8,000+ based on location[1],[2]. Neuropsychologists focus on the relationship between brain and behavior and are a type of clinical psychologist, meaning they have received advanced training/education[3],[4],[5]. As needed, they will refer students to other specialists to perform non-LD tests (e.g., tests for hearing or speech issues).
Private practice evaluations are significantly more comprehensive than public schools’ because, as mentioned in Part 2, schools generally only perform tests required to identify academic-related challenges and do not consider cognitive abilities, executive functions, etc. Comprehensive evaluations are in the neuropsychologist’s best interest as having a deep understanding of the neurological processing impacting the student’s functioning is key to building an effective treatment plan. For neuropsychologists, getting students on the right treatment plan is critical to building the brand and trust required to grow their practice.
Chart 2: Public school vs. private practice evaluations[6]
Stage-Gate 2 – Does the student require an educational therapist? The neuropsychologist considers findings from both discussions with the family/teacher and the comprehensive evaluation to decide whether a referral to an educational therapist is necessary.
Step 5: Educational Therapy Delivered
Families will find an educational therapist to deliver educational therapy to the student directly. Before starting treatment, most educational therapists do another preliminary assessment to better understand the situation and student’s struggles.
Students receive educational therapy from their educational therapist 1-on-1 after school (virtually, in a clinic, or at students’ home). To teach students the skills that are under-developed, educational therapists use students’ school-provided assignments and create their own content based on the student needs and cognitive abilities. Instruction is often provided using the evidence-based treatment for which the educational therapist is certified, and this is where the approaches to special education from Part 1 (i.e., direct instruction via Orton-Gillingham, strategy instruction) come in.
Educational therapists also engage with schools (via teachers/case managers) and/or other specialists (e.g., psychiatrists, therapists) to ensure necessary accommodations are implemented, to better prepare for students’ upcoming assignments, and to flag any new issues.
Step 6: Progress Monitored
Progress is monitored similarly to the Public School Path; however, rather than the IEP team, the educational therapist has full goal-setting authority and reports progress to parents and the teacher/case manager.
Providers
Private practice providers are called educational therapists. Educational therapists are specialists in certain LD-related areas (e.g., dyslexia, dyscalculia) whereas special education teachers are generalists focused on serve the broader needs of the classroom.
Rather than being employed by schools, educational therapists run their own or work for an educational therapy (EdT) practice where they manage relationships with families directly. Because families become their paying “customers”, educational therapists will invest in specialized training/certifications (e.g., Orton-Gillingham) and/or stay more abreast on LD-related research to better serve their families. Since special educators have no paying “customer” and instead focus on serving their school’s broader LD needs, they lack the same incentives.
Nevertheless, let’s discuss key business considerations of private EdT practices.
Student acquisition
EdT practices acquire students via four channels. They get clinical referrals primarily from neuropsychologists but also from psychiatrists/therapists treating ADHD, anxiety, or autism that realize their patient needs educational therapy. They get word-of-mouth referrals from case managers at private schools or from parents of students already receiving treatment from their practice. Practices list themselves on directories used to find educational therapists (e.g., Association of Educational Therapists), and last, they perform traditional digital marketing tactics like social media posting, podcasts, blogs, etc.
Service mix
EdT practices primarily deliver educational therapy (Step 5 above), but also provide ancillary services to support families holistically.
Chart 3: Educational therapy services breakdown
Services delivered virtually are most financially favorable given lower overhead costs. Even meeting at students’ homes incurs additional costs like travel reimbursement and/or liability insurance.
Revenue model
EdT practices are managed by a ‘Practice Director’ (PD) who oversees multiple educational therapists that solely deliver “Educational Therapy Sessions”. PDs also deliver each service listed in Chart 3 above and are responsible for administrative tasks (e.g., billing, marketing, etc.).
To maintain quality and intimacy with families, practices aim for a student-to-PD ratio of ~20:1, which often can take shape by having ~5 part-time educational therapists treating ~4 students each on average[7]. Chart 4 calculates service volume based on those assumptions.
Chart 4: EdT practice volume projections
Price per-session varies by practice based on location (e.g., rural vs. urban), therapist experience/certifications, and strategy (e.g., intimacy vs. scale). Thus, it’s hard to pinpoint an average price, but Chart 5 below projects annual revenue (assuming no churn) based on pricing scenarios generated from my market research.
Chart 5: EdT practice revenue projections
Irrespective of price, with multiple sessions occurring almost weekly, educational therapy sessions are comparable to a subscription business with recurring revenue and generate a solid average revenue per-unit (ARPU) over one-year (Row E above). Practices can ramp-up revenue by adding more educational therapists (or students per therapist), but that would require hiring another PD (to keep student-to-PD ratio at 20:1).
Labor
Hiring educational therapists for an EdT practice requires being strategic about both certifications and employment classification (i.e., 1099/W-2).
Certifications[8]
Unlike “traditional” healthcare, there are currently no state licensure requirements to deliver educational therapy.
The Association of Educational Therapists (AET) does provide some academic and experience-based requirements to becoming an Educational Therapist (ET/P); however, the most marketable and effective educational therapists typically have the following:
Education-Related Degree: Either a Masters in Education or Bachelors in Special Education
Educational Therapy Certificate: 12 to 18-month university-based program offering professional certificate in educational therapy. An ‘Education-Related Degree’ is a pre-requisite.
Evidence-Based Program Training: Training in programs like Orton-Gillingham for dyslexia. This is where the “specialization” comes in!
Employment classification
Independently contracted (1099) educational therapists are compensated per-session, do not receive benefits, and pay for their technological tools (e.g., for notetaking). Therapists choose this route if they view the job as a “side-hustle”, want control over working hours, and/or want to focus solely on treating students (since the PD handles administrative tasks).
Full-time employee (W-2) educational therapists are salaried. Having “fixed cost” employees means EdT practice unit economics will be less predictable and vary based on demand. However, compared to contractors, FTEs may be more invested in the practice’s quality/success and are not compensated per-session (and thus not incentivized to maximize the number of students seen).
Nevertheless, educational therapist salary (in New York) is $93,750 (i.e., ~$75,000 plus 25% for benefits)[9] or roughly $46-47 per-hour (though 1099 therapists earn a premium). You can do the unit economics calculation based on ‘Price per Session’ from Chart 5, but please reach out if this seems particularly interesting to you.
Payers
The Private Practice Path is more comprehensive, specialized, and intimate than The Public School Path, but substantially costlier. While the IDEA places LDs in the same category of “disability” as neurological disorders like ADHD and autism, LDs are viewed as an “academic issue” by payers and are not covered whereas ADHD and autism generally are covered.
However, families can use FSA or HSA dollars for both the private practice evaluation and educational therapy if a physician/pediatrician provides a “Letter of Medical Necessity”; however, even with the FSA, out-of-pocket costs are still substantial.
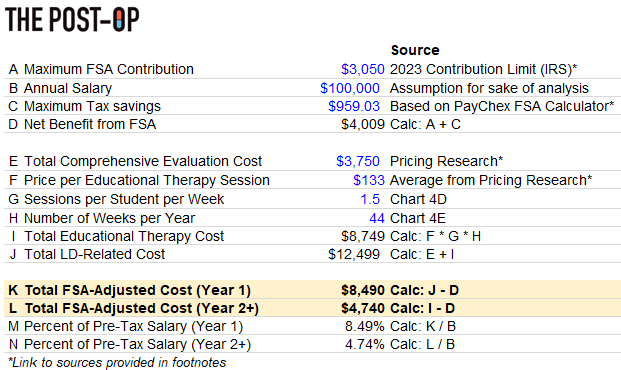
Chart 6: FSA-adjusted out-of-pocket cost analysis[10],[11],[12]
Families would pay ~$8,500 in Year 1 and ~$4,750 each year following (since the $3,750 for ‘Comprehensive Evaluation’ is only spent once). For someone making $100,000 (i.e., ~$60,000-$70,000 more than Medicaid’s eligibility limit), FSA-adjusted out-of-pocket costs still comprise roughly 8.5% and 4.75% of their pre-tax salary in Year 1 and Year 2+, respectively. Not particularly affordable!
Parting shot
By now, you likely agree the Private Practice Path is better for students than the Public School Path. So how do we make it more accessible and affordable? One option is to invest in technology that increases the availability of neuropsychologists and/or educational therapists and arms them with data to better serve students. Another option is to somehow convince insurance to cover evaluations and therapy.
We’ll unpack both options as we wrap up Season 2 the next two weeks. Stay tuned!
**
Links to: Sources | Graphics (PPT) | Analysis (Excel)
If you want to chat further about LDs or anything healthcare-related, follow me on Twitter @z_miller4 or connect with me on LinkedIn!
If you are an early-stage startup and potentially interested in my support for any unit economics or financial modeling-related activities, please fill out the form here.







Love the thoughtful unit economics analysis here - nice work Zach!