Part 4: Starting the home dialysis conversation
A closer look at the operational requirements, outcomes, and business case
Home dialysis improves quality of life for patients and offers additional payments for dialysis providers, but only 14% of ESRD patients receive dialysis at home. Here, we will unpack the operations, clinical, and business considerations of home dialysis before Part 5 goes deeper into how we can increase that 14%.
Chart 1: Utilization by type of dialysis[1]
The 14% is comprised of 2% of patients receiving home hemodialysis and 12% receiving peritoneal dialysis. Note that even DaVita and Fresenius still only deliver ~15% of dialysis at-home[2].
What is home dialysis?
Patients have two home dialysis options: home hemodialysis and peritoneal dialysis.
Home hemodialysis (HHD)
Hemodialysis (HD) is the type most performed in the clinic. As described briefly in Part 1, to perform hemodialysis, you need tubing (to create a vascular access point allowing blood to flow out of the body), a blood thinner (to keep blood from clotting while dialyzing), a pressure monitor and pump (to ensure blood pressure doesn’t get too low or high during the process), the dialyzer (to filter waste out of the blood), dialysate solution made up of water, electrolytes, and salts (to draw waste out of the blood while in the dialyzer), another pressure monitor and more tubing (both to make sure the blood properly gets back into the body). Graphic 1 below provides an illustration.
Delivering hemodialysis at home requires the patient’s home has the necessary infrastructure/overhead typically provided by outpatient dialysis clinics (i.e., water, electricity, space). Water, an element of dialysate, is the most critical as it must be “ultra-pure” (i.e., much cleaner than drinking water) and meet standards set forth by the Association of the Advancement of Medical Instrumentation[3]. Water cleanliness is critical as water can sometimes sneak from the dialysate through the fibers in the dialyzer and into the patient’s blood.
Graphic 1: How HHD works[4]
Peritoneal dialysis (PD)
Peritoneal dialysis is the other home dialysis option and does not require a dialyzer. Instead, there is an ‘exchange of dialysate’ in and out of the body – dialysate enters the peritoneal cavity through a catheter, absorbs wastes/extra fluid from the body, and is eventually drained out of the belly via the catheter.
There are two types of PD. During continuous ambulatory peritoneal dialysis (CAPD), this exchange is done manually as the patient or caregiver replaces bags of dialysate upon completion. Automated peritoneal dialysis (APD) is where a machine called a cycler does the exchange automatically 3-5x per night. With APD, patients fill 3-5 bags of dialysate into the machine (one for each exchange) and then at pre-set times while sleeping, the machine will repeat the following: release a clamp allowing solution to drain from the belly into a drain line, warm fresh dialysate before it enters the body, and then releases a clamp allowing the dialysate to flow into the body. 86% of PD patients receive APD while only 14% received CAPD[5].
Graphic 2: How CAPD & APD work[6],[7]
HHD vs. PD
Compared to HHD, PD requires less equipment, infrastructure (i.e., no dialyzer, less water supply), and caregiver support, and its treatment requirements provide greater flexibility (e.g., performed while sleeping). In addition, some believe it is favorable for patients to start on PD and transition to HD/HHD as their kidney function declines[8]. Altogether, this helps explain why PD is the most common home dialysis option (see Chart 1).
However, there are clinical and social reasons why PD may not be a fit for everyone[9]. Since PD requires the placement of a catheter in/around the abdomen, it may not work for patients with surgical scars in the abdomen, a weakened abdominal muscle (i.e., hernia), and other inflammatory abdominal processes (e.g., inflammatory bowel disease). PD also requires patients have some residual kidney function, and as alluded to above, PD patients’ kidneys will likely deteriorate to the point where HD/HHD or a transplant are required.
If PD is not a viable option, a patient could consider HHD, but as outlined, HHD is more resource-intensive and complex. So goes the vicious cycle of home dialysis.
Role of dialysis providers
Graphic 3 below outlines the various responsibilities borne by dialysis providers during the home dialysis process from beginning to end. One nuance is that some clinics (likely the ones with more resources) have “home units” with nurses and technicians only focused on supporting home dialysis patients and executing these activities.
Graphic 3: Dialysis providers’ home dialysis responsibilities [10],[11],[12],[13]
Home dialysis vs. in-clinic dialysis
Outcomes and experience
Since HHD is essentially equivalent to in-clinic HD, the question here is how PD and in-clinic HD outcomes compare. Research seems limited, but this UpToDate article is the best I could find. It essentially states that, for patients starting dialysis, PD may provide short-term survival benefits, but survival may become comparable to or even worse than in-clinic HD after the first few years.
On the other hand, and arguably undeniably, the HHD and PD experience improves patients’ quality of life as well as their mental health. Rather than 4+ hours in the clinic 3-4 times per week, patients can dialyze more frequently, but for shorter periods of time (i.e., 2 hours, 5-7 times per week) or while asleep[14]. This even provides patients the flexibility to travel! Fresenius reported it saw a 20-point increase in satisfaction scores from home dialysis patients compared to those receiving in-clinic dialysis[15].
Patient care costs
On a per-treatment basis, home dialysis is less costly to deliver than in-clinic dialysis! Home dialysis requires significantly less labor as labor is only needed for training patients/caregivers upfront, facilitating the ongoing check-ins, and occasionally monitoring patients remotely. The labor hours required for these activities pale in comparison to the labor hours needed to administer dialysis in the clinic for 18 hours a day, 6 days a week. In addition, there are also fewer overhead costs attributable to home dialysis.
Altogether, anchoring on a Prima Health Analytics analysis, my best estimate of the variable cost to deliver home dialysis is $230 (see quick calculation here) compared to $270 for in-clinic dialysis as calculated in Part 3 (Chart 6, Row D). My pseudo-hot take is that $230 is a fairly conservative estimate.
Reimbursement
In theory, dialysis providers get reimbursed more for home than in-clinic dialysis[16]. They receive the same bundled ESRD PPS rate ($257.90 in 2022), and the amount reimbursed for home dialysis each week must be equivalent to one week of in-clinic dialysis (i.e., 3 sessions worth)[17]. There are also two home dialysis specific add-ons to the ESRD PPS rate.
The first add-on is the Transitional Add-on Payment Adjustment for New and Innovative Equipment and Supplies (TPNIES), which provides an additional payment for “approved” HHD or PD machines used during home treatment[18]. My understanding is that these machines cost ~$15,000 and ~$7,500, respectively[19]. Only the Tablo HD machine from Outset Medical has been approved for TPNIES to-date, but since more patients receive PD than HHD, let’s assume a $7,500 PD machine with remote monitoring capabilities for the sake of the analysis. Nevertheless, using the TPNIES calculation methodology found here, said PD machine only results in a $1-2 add-on per treatment. My calculation can be found here, and you’ll notice the add-on (Row R) grows only if more expensive machines are used (e.g.,~$15,000 HHD machine generates a $9-10 add-on per treatment).
The second add-on is reimbursement for nursing time spent training patients and is worth $95.60 per training session[20],[21],[22]. Assuming patients receive an average of ~10 HHD and/or PD training sessions, $95.60 per session is ~$956 in additional revenue per patient (i.e., $95.60 * 10 = $956). Spread across 156 treatments per year, this comes out to a training add-on per treatment of ~$6 (i.e., $956 / 156 = ~$6.13).
The business case
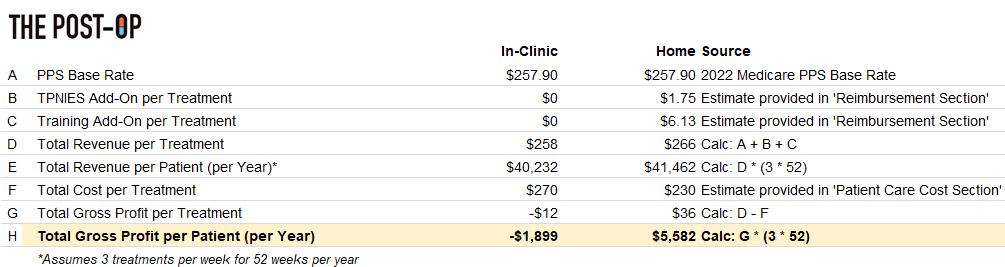
Tying everything together, despite limited incremental benefit from add-on payments (Rows D & E), Chart 2 below illustrates how home dialysis variable costs (Row F) are still low enough to generate a positive gross profit (Row H).
However, sadly, given their small size and current restrictions, the CMS add-on payments are not yet ‘low-hanging fruit’ for providers hoping to broaden home dialysis offerings. Instead, the business case relies upon lowering variable costs to generate positive gross profits, and that can be operationally challenging to achieve in practice.
Chart 2: Medicare revenue and gross profit comparison – in-clinic vs. home dialysis
Parting shot
Regardless, for providers, home dialysis done right can turn Medicare patients into a profit generator and for patients, it offers a vastly superior dialysis care experience. Together, I believe this alignment of incentives has the potential to eventually provoke a tectonic shift in the provision of care for ESRD patients.
So… *cue suspenseful music*
Come back next week as we’ll discuss both obstacles to and solutions for increasing home dialysis utilization!
***
Links to: Sources | Analysis (Excel)
As always, follow me on Twitter @z_miller4 or connect with on LinkedIn here! Would love to chat if you’re interested in kidney care, digital health, etc.
Note: This article was edited on November 3rd to reflect an updated value of $95.60 for the training add-on. I apologize for any confusion and thank you Eric Weinhandl for the call-out








Hello! The big providers are aiming to get 25% of patients on home, but the issue is largely on the patient side. There's a lot of requirements on behalf of the patient and/or caregiver (from being able to lift heavy boxes to not having pets that can create infection risks) that causes many patients not to choose home care. The financial incentives are very significant for dialysis providers, especially in the value based arrangements (CKCC).
What is included in the bundled payment? Any meds like iron, phosphate binders, Vitamin D, etc?