Part 1: What is end-stage renal disease (ESRD)?
Its impact on the body, treatment options, and most importantly, reasons why you should care
Your kidneys, chronic kidney disease (CKD), and ESRD[1]
ESRD is the fifth and final stage of chronic kidney disease or CKD. Key to understanding ESRD (and part of the ethos of The Post-Op) is first learning what a kidney is and its role in the body. Each person has two kidneys, which are bean-shaped organs located below your ribs and towards the middle of your back. Your kidneys remove liquid waste from the blood in the form of urine. They also balance the chemicals such as salt and other substances (e.g., phosphorus or calcium) in your blood. Each kidney has roughly one million nephrons, which are tiny filtering units that remove the waste.
The desk drawer analogy helps explain kidney function. If you need to clean a desk drawer, you could either 1) open the drawer and start picking out the stuff you need or 2) dump everything out of the drawer and then put the stuff you need back in the drawer. Option 2 is more efficient and that is how kidneys clean your blood. Blood is dumped into the nephron and the “stuff you need” is pulled back into the blood vessel (where salt, water or minerals are added as needed) while the rest (i.e., waste) becomes urine[2].
Graphic 1: How kidneys work[3]
In addition to removing waste, kidneys also produce three important hormones: renin (regulates blood pressure), erythropoietin (needed to make red blood cells), and active vitamin D (absorbs calcium from food).
CKD means your kidneys are damaged and as a result, are not properly doing the various jobs I described. The inability to do each of those jobs has unique implications[4]:
Unable to remove waste from blood: Puts too much strain on the heart and blood vessels, which can lead to high blood pressure, heart disease, or stroke
Unable to regulate substances like phosphorus or calcium: Builds up potassium, which can result in irregular heartbeats, and pulls calcium from the bones which weakens them and can lead to bone disease
Unable to produce red blood cells: Inhibits ability to deliver oxygen throughout the body (a function of red blood cells) and can lead to anemia, a condition where your body lacks the requisite amount of blood cells
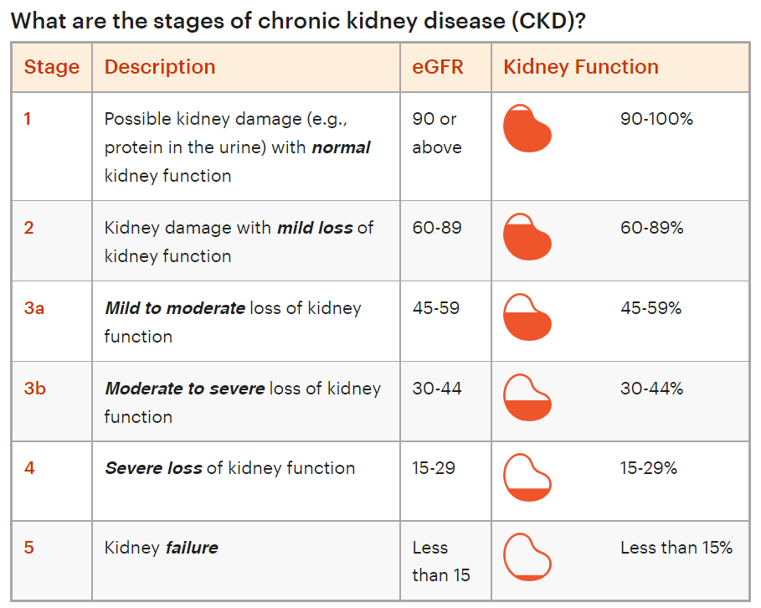
Last, to contextualize, CKD has five stages, the last of which is ESRD (also called kidney failure). The stages are determined by the result of an estimated glomerular rate (eGFR) test, a blood test that most commonly measures the level of creatinine (i.e., a toxin/waste product) in your blood. Healthy kidneys filter creatinine out of your blood like in the desk drawer analogy, but when one has kidney disease, creatinine stays in the blood and gradually builds up, making it a good proxy for kidney function. Creatinine levels in general can vary person-to-person, so the final eGFR also accounts for age, sex, race, etc.[5]
Chart 1: Stages of CKD[6]
How is ESRD treated?
As discussed, once a patient is diagnosed with ESRD, their kidneys lose the ability to filter blood altogether and either dialysis or a kidney transplant is required to stay alive. In 2020, 71% of ESRD patients received dialysis while 29% received a kidney transplant[7].
The goal of dialysis is to remove waste from a patient’s blood by filtering it, and there are two different types: hemodialysis and peritoneal dialysis. During hemodialysis, the patient’s blood flows from a vein or artery (called a dialysis access point) into a machine (called a dialyzer), which then mixes with a fluid (called dialysate) to remove waste from the blood and return it to the body. Peritoneal dialysis does not require a dialyzer, but instead, the dialysate flows into patient’s abdomen via a catheter, absorbs waste, and then is subsequently filtered out of via the catheter.
Dialysis can be delivered at a dialysis clinic, at home, or in the hospital. Hemodialysis is more common and is primarily delivered in the clinic or hospital whereas peritoneal dialysis is primarily delivered at home. Patients receive in-clinic dialysis roughly three times per week and each session lasts 3-5 hours. The treatment regimen for home dialysis varies as it can be done daily for shorter increments of time, at night while you sleep, or three times per week for 3-5 hours (like in the clinic).
Kidney transplants are more self-explanatory. It is the procedure where a healthy kidney from a deceased or living donor is placed into an ESRD patient, and it generally leads to superior outcomes compared to dialysis. A bit more to come in Part 2 on transplants.
So, why should you care?
Regardless of background (investor, operator, clinician, advisor, product builder, etc.), I believe there are diverse reasons to spend time better understanding ESRD.
Market size: The market is unique in that is huge, but patients only have two options for treatment.
Prevalence: 37M people in the United States have CKD[8], nearly 800,000 of which have progressed to ESRD and require dialysis or a kidney transplant to survive[9]. For context, 800,000 is 50-100K more people than the populations of “up-and-coming” cities like Seattle, Denver, and Nashville. There are also meaningful differences in prevalence based on patient ethnicity (outlined below).
Chart 2: ESRD prevalence by patient ethnicity[10]
Spend: Total Medicare fee-for-service (FFS) expenditures alone (not even including Medicare Advantage or commercial insurance) for ESRD totaled $37.3B in 2019, accounting for more than 7% of the $522B Medicare spent that year despite ESRD patients comprising less than 1% of the total Medicare population[11]. We pay 1.45% of our paycheck in taxes for Medicare each year[12], so if 7% goes to ESRD specifically, then 0.1% (= 1.45% * 7%) of every paycheck is technically used on dialysis or kidney transplants!
Experiences needing fixing: Both methods of treating ESRD are imperfect and will be discussed further in later parts.
Dialysis: ESRD patients require dialysis to stay alive, but the experience is time-consuming and emotionally draining. 87% of those receiving dialysis do so in the clinic, meaning they are spending 12+ hours a week in a dialysis clinic (i.e., 3 sessions per week, 4 hours per session). The average life expectancy on dialysis is only ~5 years[13], and in addition, various studies have also shown the adverse effects dialysis can have on mental health[14].
Kidney transplants: Kidney transplants are the most effective form of treatment for ESRD but are plagued by vast supply and demand imbalances. In 2021, there were ~90,000 patients on the kidney transplant waitlist, but only ~24,000 transplants were performed. This transplantation rate pales in comparison to the next most in-demand organ, the liver, where there were 12,000 patients on the waitlist and 9,000+ transplants performed[15].
Unique regulatory environment: In 1972, given the prevalence of ESRD and the cruciality of access to treatment (survival!), Medicare extended coverage to all ESRD patients. Fast forward to today, since Medicare still bears much of ESRD costs, the Centers for Medicare & Medicaid (CMS) and the Center for Medicare & Medicaid Innovation (CMMI) have shown a willingness to at least experiment with alternative and value-based payment models within ESRD. I view this as a unique tailwind since many ESRD-related businesses have thus already dabbled with value-based care.
Parting shot
Ultimately, preventing CKD from progressing to ESRD is the goal. However, given the prevalence of CKD (37M people as mentioned), its complexity (commonly comorbid with heart disease and diabetes)[16], and general challenges slowing CKD’s progression, ESRD is unfortunately not going away anytime soon. With that in mind, the subsequent parts of this mini-series will dive deeper into both the basics and nuances of ESRD and hopefully facilitate discussion and innovative thinking in an area in need of a closer look.
***
Links to: Sources (footnotes are also linked) | Graphics (PPT)
Follow me on Twitter @z_miller4 or connect with me on LinkedIn here! Always down to chat with other folks interested in the space.